Linear accelerators, LINAC, are large scaled medical devices that deliver external radiation in the form of a beam to cancerous tumors in order to shrink them. As with most medical equipment, LINAC systems are expensive which is a barrier that many facilities face when purchasing a new or refurbished unit.
With the expense of these large scaled systems it is important to make sure they are properly maintained and that you have access to linear accelerator parts for repair as needed. Medical facilities can contract with companies that specialize in maintenance and repair services of LINAC systems such as Acceletronics or have on staff a team of professionals whose job it is to provide these services for their equipment. There are advantages and disadvantage to both options, facilities choose based on their budget and facility needs.
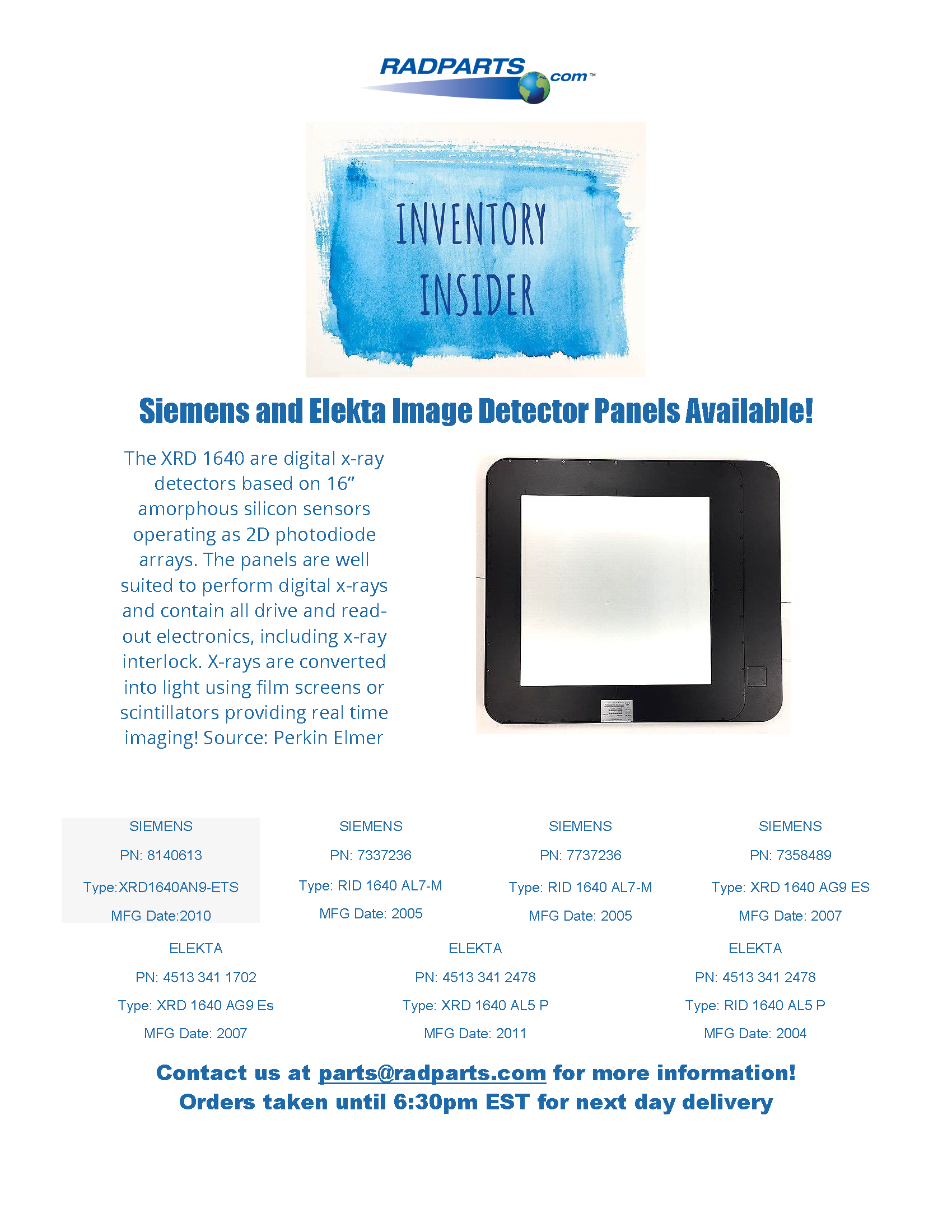
Linear accelerators have evolved over the years. LINAC machines no longer only provide external radiation beams for treatment. Major advancement in this technology include onboard imaging systems and portal dosimetry. Such complex systems require biomedical and clinical engineers to not only understand what these machines do but also how they are operated. Even with advanced training, until the engineer has hands on experience it is difficult to truly understand how the machine functions.
Not only is the linear accelerator expensive but the expertise to use and understand the machine is costly as well. This again is an issue that faces many medical facilities. These two factors alone make up the most significant aspect of expense faced by facilities when deciding on the purchase of equipment.
All linear accelerators are not created equally and therefore when replacing an existing system there will be a significant cost to not only bring new equipment in but also the training on the individual piece of equipment. One way to combat this is to replace existing LINAC with identical refurbished linear accelerators.
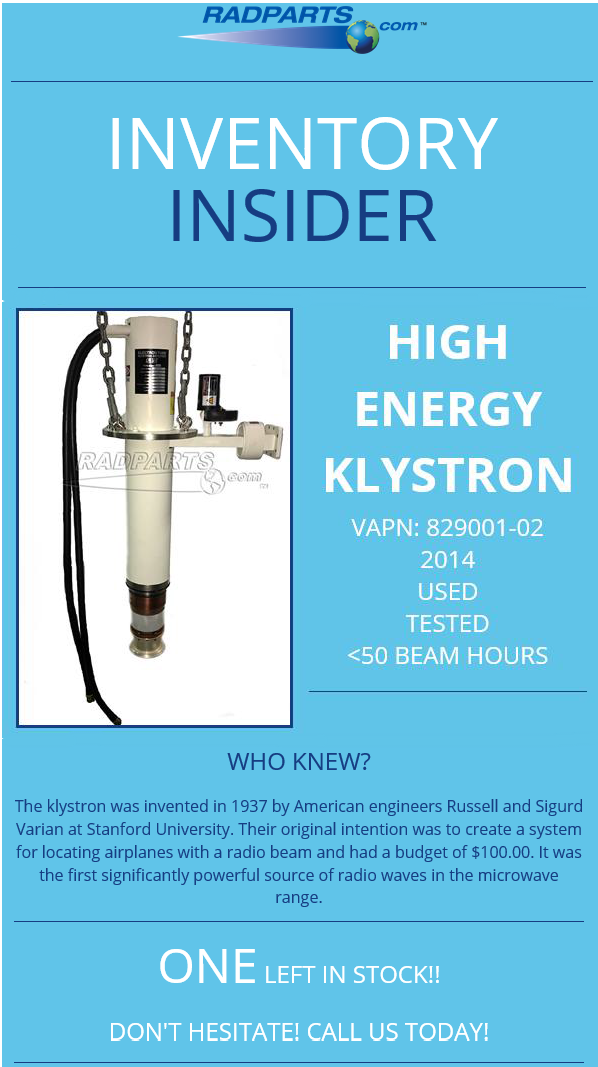
We have discussed a lot about the expense of these units however there is also significant revenue to be gained by having external radiation treatment available to patients seeking treatment for cancerous tumors. It is important for facilities to make sure these machines are functioning at peak capabilities at all times. Downtime not only impacts revenue but also patient care. In order for patients to have effective treatment for their tumors it is important they are able to strictly follow the treatment schedule laid out by their radiation team. If equipment is down this is not possible.
To ensure that patient care and revenue is not affected by machine downtime it is crucial to maintain equipment. Machine maintenance includes repairs in anticipation of failure. If a parts failure is eminent based on previous experience it behooves the facility to purchase the LINAC replacement part ahead of time so that service can be provided around patient’s treatment schedules. This allows facilities to schedule downtime to prevent unplanned downtime.
Radparts is the world’s largest independent distributor of OEM replacement parts for Linear Accelerators and Radiation Oncology equipment. Radparts provides high quality, user friendly, low cost parts support for linear accelerators and radiation equipment. More information can be found at https://www.radparts.com/.